- Home
- Patients
- Patient Information
- Nerve Root Pain and Some of the Treatment Options
Nerve Root Pain and Some of the Treatment Options
Introduction
Nerve root pain comes from a nerve in the spine. Nerves carry messages about sensations and control of muscles and so disorders of nerves can cause pain, numbness, increased sensitivity or weakness of muscles. The pain is often felt in the area of the body supplied by that nerve. It is common for the leg nerves and arm nerves to be affected.
Lumbar nerve pain (often called ‘sciatica’) generally goes below the knee. Back pain is usually felt between the lower ribs and the buttocks. Often there will be a combination of back and leg pains. In sciatica the leg pain is worse than the back pain. Sciatica is usually caused by a disc prolapse (a ‘slipped disc’), but there are other causes.
Brachial neuralgia (nerve pain in the arm) is very similar to sciatica but comes from the neck nerves. Sometimes the pain goes down the arm as far as a specific finger.
‘Radicular pain’ is a term doctors use to describe pain when it is mainly from a single nerve root.
If you have been diagnosed as suffering with such a problem, this gives you the best and most up to date advice on what to expect and how to manage it.
This information is for those who have mainly nerve pain rather than back pain. Often nerve pain and back pain are present at the same time. If the limb pain is worse than the back pain it is more likely to be from the nerve.
‘The Back Book’ is an excellent source of information about back pain and should be available from your GP.
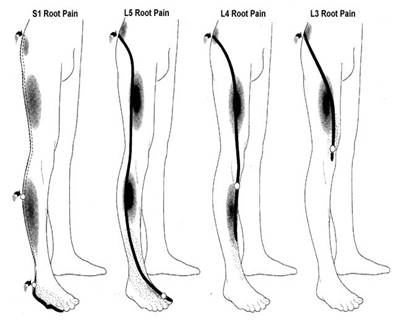
Some common patterns of Nerve root pain in the leg
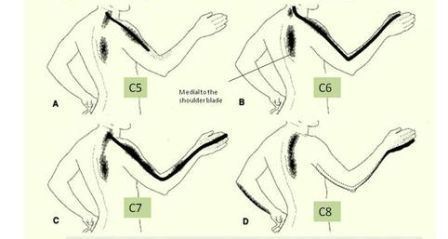
Some common patterns of Nerve root pain in the arm
Some Important Facts
In patients attending general practice for the first time with sciatica 75% are better within 28 days.
The most common age for sciatica is 35-40. It is less common as you get older.
If an episode of sciatica settles there is about a 90% chance it will not happen again in the next ten years.
Certain types of disc prolapse are more likely to recur than others.
The main risk factors for sciatica are inherited, and you can’t choose your parents!
Regular exercise may reduce the risk of nerve root pain, or at least delay it’s onset. sedentary occupations are more at risk than those involving activity.
Being very overweight is another risk factor.
Surprisingly, heavy manual work and repetitive lifting do not seem to be risk factors for sciatica.
The Main Things About Nerve Root Pain
Pain spreads into the leg or the arm, generally below the knee or the elbow.
The pain is often associated with altered sensations, such as pins & needles, burning or numbness.
Coughing and sneezing can make the limb pain worse. We call this ‘Impulse’ pain
The limb pain is the main or dominant pain compared to the back or neck pain.
The diagnosis of nerve root pain can sometimes be clear and simple , but sometimes can be quite a difficult judgement. Please try and resist the tempatation to self diagnose on the Internet ! . You might be right, but you might not. Allow your Health Care Professional to listen to your story regarding how the pain started, what it is like and what is happening to it now. That way the two of you can come to a diagnosis.
What is a prolapsed disc?
The intervertebral discs have a jelly centre, (the pulposus) which can ooze its way out through a tear in the strong gristle of the disc (the annulus).
The jelly then irritates and compresses the nearby nerve root causing pain in the area of the limb which the nerve supplies.
 Most people get better
Most people get better
Fortunately most episodes do not last long. Medications and therapies can help but there isn’t usually a “quick fix”. There is a need to wait for natural recovery to take place. Most patients are improving well by 6 weeks from the start of the symptoms into the limb.
By 13 weeks the majority of patients are much improved and virtually back to normal, but low grade symptoms may sometimes persist for several months.
If the pain isn’t getting better or is really affecting your ability to get on with life and more than four weeks have gone by then that is the sort of time to be thinking about seeing a specialist. That might be a surgeon, a specialist nurse or someone who can advise about the ‘next steps’.
If the pain ‘centralizes’ (that is, it goes out of the limb and more towards the spine) this is a good sign of improvement. Symptoms of numbness or weakness may last longer than the pain.
Healing
When a disc prolapses (or ‘slips’) it no longer has its normal nutrition and so usually shrinks quite quickly.
Imagine a piece of moist crab meat left on a plate; it would soon shrivel up and shrink away. That is what often occurs with a disc prolapse.
The part of the disc that is left behind will often repair itself.
As you get older your discs become stiffer with less jelly, which is why disc prolapses are less common in older people.
The best way to deal with the problem is to exercise sensibly, stay active, avoid being overprotective, and to lead as normal a life as possible.
DO take painkillers so that you can get on with your life
Diagnosis
In the initial stages most patients only need to see their GP. The diagnosis is made largely from the symptoms and the initial examination.
Here are some of the common examination findings: –
Spinal movements produce limb pain e.g. in lumbar nerve root pain (‘sciatica’) bending down to touch your toes causes the pain to go to the leg.
In brachial neuralgia (nerve root pain in the arm) turning the neck towards the painful side can increase the arm pain.
Nerve stretching tests cause pain to down the limb.
Simple tests of the function of the nerve by a health care professional e.g. power, reflex and sensory tests, will help identify which nerve is likely to be the one that is causing the pain.
Nerve root pain can be very varied, the amount of pain is NOT related to how large the disc is, and varies a lot. Distress and fear can often make pain worse. Quality information about the facts of sciatica is important to help understand how best to deal with it.
Most sciatica gets better, the only situation that is considered an emergency is when there is numbness between the legs or difficulty with bladder or bowel control.
LOSS OF SENSATION BETWEEN THE LEGS AND AROUND THE BUTTOCKS WITH LOSS OF CONTROL OF THE BOWELS OR BLADDER IS AN EMERGENCY – IT IS RARE, BUT IF IT OCCURS PHONE 999 OR SEEK QUALITY MEDICAL ADVICE QUICKLY
M.R.I. Scanning
An MRI scan gives an excellent picture of the internal structure of the body. It does not involve x-rays and is very safe. It is quite noisy and some people find the scanner claustrophobic.
In the early stages the use of scans to locate the problem is not normally required. A scan may be helpful when the pain is not settling or an intervention like an injection or operation is being considered.
We ‘treat the man not the scan’ and so if the sciatica looks as though it will settle without interventions then a scan is not required.
Scans are very sensitive and will detect almost all serious spine problems such as cancer, infection or pressure on the spinal cord or spinal nerves. The scans will often detect minor abnormalities that may not be important. Statements such as ‘Wear and tear changes’ can be a worry for some people. Doctors tend to view ‘degenerative change’ or ‘wear and tear’ as a part of normal ageing, like developing grey hair.
X-RAYS
Spinal x-rays provide only limited information in cases of nerve root pain and are therefore not requested routinely.
Drug Treatments
Medications are used to help with the pain and can improve your quality of life whilst healing take place.
Effective drugs include non-steroidal anti-inflammatory drugs, pain relieving drugs, nerve pain relieving drugs, and the short term use of muscle relaxation drugs if spasm is present.
Not all of these medications are always needed. Exact decisions about what you need are the role of your GP/Hospital Doctor. Often a combination of different medications, taken regularly, provides an umbrella of pain relief. This is more helpful than just taking tablets when the pain is really bad. It is easier to keep pain away rather than trying to get rid of it once it is established.
One type of medication from each of the three main groups can be combined with medication from the other groups
Anti inflammatories: Non-steroidal anti inflammatory drugs (NSAIDs)
Such as Ibuprofen 400mg three times a day OR Diclofenac 50mg three times a day. Short course of up to six weeks are safe. If gastric side effects occur (5% or less) this can be treated with effective acid reducing medication. There are some other anti-inflammatory tablets they may also be tried.
Simple analgesics: Paracetamol 1G six hourly OR co-codamol Two six hourly. Co dydramol Two six hourly
Stronger analgesics: Sometimes ‘top up’ medication for breakthrough pain will be necessary. Codiene or tramadol
Nerve pain medication: Amitryptiline 25 mg at night OR Gabapentin 300mg three times daily can be very helpful, particularly in combination with the other types of pain relief. These doses can be increased but only as recommended by your doctor.
Physiotherapy & Manual Therapies
Assessment and good advice regarding reassurance and how to best manage can be very helpful. In some cases manual therapy may increase the symptoms or not help greatly. Most physical therapists would tend to wait until some of the pain has settled before trying certian types of mobilisations.
If most of the limb pain has settled then such treatment can be very helpful and considered in order to ease any residual stiffness, and to progressively reactivate and rehabilitate back to full function.
Certain exercises can sometimes be very helpful , ‘McKenzies’ exercises seem to help the pain to come out of the leg in some patients.
Some treatments do not seem to have scientific evidence to support their use. Electrical therapy, acupuncture, ultrasound and traction do not seem to be helpful.
Injection Therapy
Injection therapy is usually only required if the problem is not settling satisfactorily after an appropriate period of time.
These treatments can be delivered by a variety of specialists, including Rheumatologists, Pain Management Anaesthetists, Radiologists and Orthopaedic surgeons.
The two injection techniques most often employed are
Epidural injections into the space around the nerves in the spine and within the spinal canal.
Nerve root canal injections which are more specific to the affected nerve and which require X-ray control to locate where the irritated nerve exits the spine.
Both injection techniques have the same aim, which is to relieve the pain and inflammation in the nerve while natural healing continues. They can be repeated if required. Both methods seem equally safe. Complications are uncommon, but can include infection or damage to nerves or blood vessels.
Surgery
The majority of patients get better without surgery. Often the pain will settle with time.
Surgery can be very helpful if the pain doesn’t settle with simpler measures. An operation is the most reliable way to reduce the leg pain quickly, but surgery does have some associated risks.
The results of surgery depend on the exact clinical picture and some patients may not be suitable.
Surgery is for the pain in the leg. It does not seem to alter the chance of future attacks of sciatica. It is better for pain than numbness or weakness. Numbness doesn’t usually cause many problems.
The Spine Patients Outcome Research Trial (SPORT) was an American study that has vast amonts of patient information. Click on this link if you need more information. There is the SPORT guide to non -operative care and the SPORT guide to surgery.
After surgery, 75% of sciatica patients are very much better. 20% are improved but have some minor persisting symptoms. About 5% of patients are not helped and about 1% may even be worse off.
Complications can occur and include general complications that can occur with any operation and specific complications related to the spine.
A dural tear is when the lining of the spinal canal is disrupted. It can result in a leak of spinal fluid. This happens in about 3% of operations. It doesn’t usually lead to any long term complications.
Infection can occur but is rare. Damage to nerves and blood clots in the spine or lungs can occur. See the BASS audit presentation under download files
Serious complications such as death or paralysis can also occur but fortunately are rare. A catastrophic complication of this type might occur with a risk of 1 per 400 or 500 cases. Each individual should discuss the risks and benefits of operative and non operative treatment with the surgeon.
At operation the part of the disc irritating the nerve root is removed. Usually the operation involves an overnight stay in hospital.
A recent study from Sweden of 25000 surgical cases found a risk of only 7% of a further operation for sciatica within 10 years of the first. The same risk as without surgery.
After The Operation
We usually advise you to mobilise quickly. There are good studies that show an early return to activity and wrk gets you better quicker and produces a better outcome longterm.
You should be back to full unrestricted activity at 12 weeks, including heavy manual work and contact sports.
Generally you should be safe to drive when you are able to walk briskly for about 400 yards (usually at about two to three weeks post op.)
General Advice: DO'S
Take a regular umbrella of pain relief to control the pain. Anti-inflammatory medication can be very helpful and should be used if possible.
Pay attention to posture; any position that relieves the leg pain is good.
Stay as active as possible; rest does not speed recovery.
Stay at work or return back as soon as possible. It will hurt whether or not you are working, and normal activities will not delay recovery.
Distract yourself from the pain; leisure activities, work or things you enjoy help to take your mind off the pain and fewer painkillers may then be required.
General Advice: DON'TS
Don’t be frightened of the pain. (hurt does not mean harm).
Don’t give in; doing less leads to weakness and stiffness.
Don’t panic if you have an increase in your pain; small set backs during the healing period are quite common.
Key Points
Nerve root pain usually settles over time.
Medications and adjustments in lifestyle can help to improve your quality of life while healing occurs.
Only a small number of patients who are not settling over the usual time scale needs to go to hospital for tests and other interventions.
Most disc problems heal over time and recurrence is rare.
The fitter you are the less likely it is to affect you in the future
Useful Information Sources
Patient line - The Spine Society of Europe information on sciatica.
Available in different languages and with different opinions on treatment options.
Author: McKenzie R
Publisher: Orthopaedic physical therapy Products, Spinal publications Ltd
New Zealand
ISBN095 77466 1
The Neuropathy Trust - Information and resources for patients with nerve pain, particularly that radiating into a limb.
This material was based upon that provided by:
- Mr Philip Sell – Consultant Orthopaedic Surgeon
- Dr Steven Longworth – General Practice and Musculo-skeletal Specialist
- Mr John Haynes – Spine Specialist Physiotherapist
.jpg)